Correlation between leukocyte phenotypes and prognosis of amyotrophic lateral sclerosis
Curation statements for this article:-
Curated by eLife
Evaluation Summary:
Cui et al. colleagues carried out a longitudinal analysis of blood cell counts in a cohort of patients with ALS patients. They found increased numbers of neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not with rate of disease progression. In addition, increased levels in NK and central memory TH2 T cells correlated with a lower risk of death, while increased levels of CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death. These findings have broad implications for ALS pathogenesis and the development of immune-based ALS therapies tailored to specific immune cell populations.
(This preprint has been reviewed by eLife. We include the public reviews from the reviewers here; the authors also receive private feedback with suggested changes to the manuscript. The reviewers remained anonymous to the authors.)
This article has been Reviewed by the following groups
Discuss this preprint
Start a discussion What are Sciety discussions?Listed in
- Evaluated articles (eLife)
Abstract
The prognostic role of immune cells in amyotrophic lateral sclerosis (ALS) remains undetermined. Therefore, we conducted a longitudinal cohort study including 288 ALS patients with up to 5-year follow-up during 2015–2020 recruited at the only tertiary referral center for ALS in Stockholm, Sweden, and measured the levels of differential leukocytes and lymphocyte subpopulations. The primary outcome was risk of death after diagnosis of ALS and the secondary outcomes included functional status and disease progression rate. Cox model was used to evaluate the associations between leukocytes and risk of death. Generalized estimating equation model was used to assess the correlation between leukocytes and functional status and disease progression rate. We found that leukocytes, neutrophils, and monocytes increased gradually over time since diagnosis and were negatively correlated with functional status, but not associated with risk of death or disease progression rate. For lymphocyte subpopulations, NK cells (HR= 0.61, 95% CI = [0.42–0.88] per SD increase) and Th2-diffrentiated CD4 + central memory T cells (HR= 0.64, 95% CI = [0.48–0.85] per SD increase) were negatively associated with risk of death, while CD4 + effector memory cells re-expressing CD45RA (EMRA) T cells (HR= 1.39, 95% CI = [1.01–1.92] per SD increase) and CD8 + T cells (HR= 1.38, 95% CI = [1.03–1.86] per SD increase) were positively associated with risk of death. None of the lymphocyte subpopulations was correlated with functional status or disease progression rate. Our findings suggest a dual role of immune cells in ALS prognosis, where neutrophils and monocytes primarily reflect functional status whereas NK cells and different T lymphocyte populations act as prognostic markers for survival.
Article activity feed
-

-

Author Response
Reviewer #1 (Public Review):
Cui and colleagues have performed a longitudinal analysis of blood cell counts in a cohort of ALS patients. The major findings include increases in neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not disease progression rate. Increases in NK and central memory TH2 T cells correlated with a lower risk of death, while increased CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death.
Strengths of the study include the sample size and effort to broadly include data.
Thank you for the positive comment.
Limitations of the study include indication bias, as the authors acknowledge, because the timing of the blood draws is not predefined. The specific review for possibility of infection does not, in this reviewer's opinion, …
Author Response
Reviewer #1 (Public Review):
Cui and colleagues have performed a longitudinal analysis of blood cell counts in a cohort of ALS patients. The major findings include increases in neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not disease progression rate. Increases in NK and central memory TH2 T cells correlated with a lower risk of death, while increased CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death.
Strengths of the study include the sample size and effort to broadly include data.
Thank you for the positive comment.
Limitations of the study include indication bias, as the authors acknowledge, because the timing of the blood draws is not predefined. The specific review for possibility of infection does not, in this reviewer's opinion, sufficiently address this potential for bias. Also concerning is the fact that half the subjects have only a single measurement, and how well the findings generalize to more or late measurements is not clear. Similarly, the number of later measurements driving some of the main findings is much lower, further raising concern about the potential bias. Given these issues, one really would want to see disease controls, and how the different cell counts change in another disease. Finally, there is not discussion about how or whether treatments, or changes in treatment, could influence observed counts.
We agree with the reviewer regarding indication bias and that is precisely why we performed the sensitivity analyses including 1) restricting the analysis to the first cell measure of each patient and 2) excluding cell measures with signs of ongoing infection at the time of blood draw. Reassuringly, both analyses provided rather similar results as those of the main analysis. We also agree with the reviewer regarding the varying numbers of measurements between patients. This is an unavoidable challenge to any longitudinal study of ALS patients, primarily due to the high mortality rate of this patient group. We have now added this limitation to the discussion:
“First, the main cohort was heterogeneous in terms of the numbers of cell measurements and the time intervals between measurements, as the timing of blood sampling was not predefined. Indication bias due to, for example, ongoing infections might therefore be a concern. The sensitivity analysis excluding all samples taken at the time of infections provided however rather similar results. Further, the longitudinal analysis of cell counts should be interpreted with caution because not all patients contributed repeated cell measurements. This is however an unavoidable problem for any longitudinal study of ALS patients, given the high mortality rate of this patient group. Regardless, when focusing on the first cell measures, we obtained similar results as in the main analysis.”
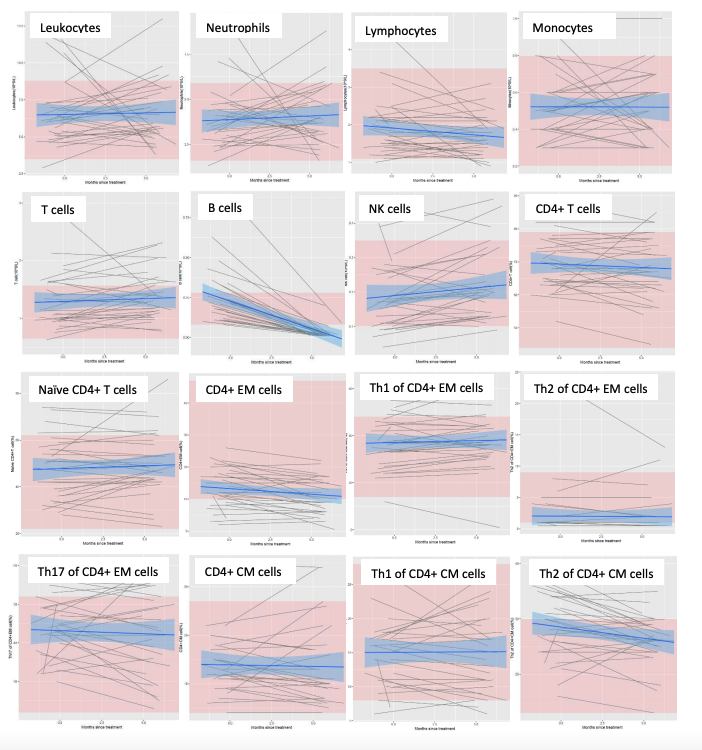
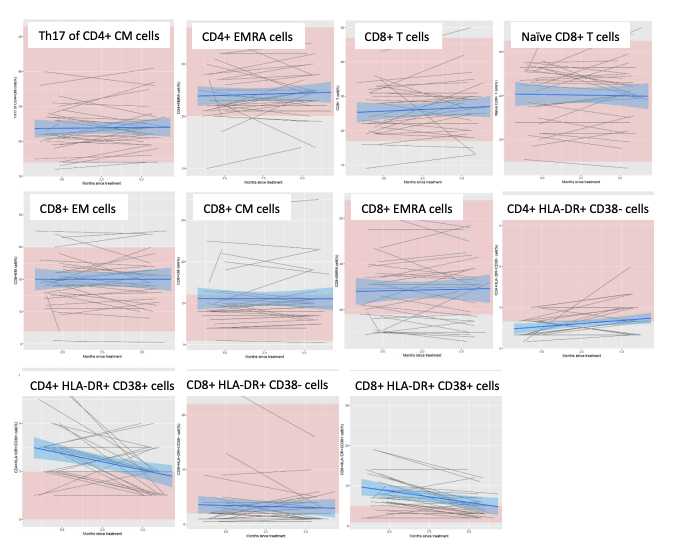
We further agree with the reviewer regarding the use of disease control. We have access to a cohort of patients with relapsing-remitting MS (RRMS) treated by rituximab (n=34), who had been measured with all the studied cell populations at the start of treatment and the 6-month follow-up. These cell measurements were processed during the same time-period using the identical setup at Karolinska University Hospital as the ones studied in the present study. In brief, we found different longitudinal changes of the studied immune cell populations between RRMS patients and ALS patients (please see below figure for details). The declining B cells are most likely due to rituximab treatment.
Given the largely different disease mechanisms, phenotypes, and treatments between RRMS and ALS, we are not confident that RRMS would be a good disease control for the present study. We are certainly willing to reconsider our position if the reviewer and editors would disagree with us. We have regardless now added discussion about this in the manuscript:
“It would therefore be interesting to compare ALS with other diseases, especially other neurodegenerative diseases, regarding the studied cell counts, in terms of both their longitudinal trajectories during disease course and their prognostic values in predicting patient outcome.”
Finally, we agree that it is interesting to consider treatment in the analysis of cell counts. Among the ALS patients of the main cohort, majority (89.6%) were treated with Riluzole. We have now added a supplementary figure to demonstrate the leukocyte counts before and after start of Riluzole treatment. The corresponding analysis is however not possible for the FlowC cohort as majority of the patients started Riluzole treatment around time of diagnosis and almost all measurements were taken after Riluzole treatment. Th17 of CD4+ CM cells CD4+ EMRA cells CD8+ T cells Naïve CD8+ T cells CD8+ EM cells CD8+ CM cells CD8+ EMRA cells CD4+ HLA-DR+ CD38- cells CD4+ HLA-DR+ CD38+ cells CD8+ HLA-DR+ CD38- cells CD8+ HLA-DR+ CD38+ cells.
We have now added this analysis to Methods and Results, including a new Figure 1—figure supplement 2.
“To evaluate whether ALS treatment would influence the cell counts, we further visualized the temporal patterns of differential leukocyte counts before and after Riluzole treatment.”
“The levels of leukocytes, neutrophils and monocytes increased, whereas the levels of lymphocytes decreased, after Riluzole treatment, compared with before such treatment (Figure 1—figure supplement 2).”
Reviewer #2 (Public Review):
Cui et al. investigated the correlation of immune profiles in ALS patients to functional status (by ALSFRS-R score), disease progression (rate of ALSFRS-R decline) and/or risk of death (or invasive ventilation use). The study longitudinally assessed basic immune profiles from a large cohort of ALS patients (n=288). Additionally, they deeply immunophenotyped a subset of ALS patients (n=92) to examine immune cell subtypes on ALS status, progression rate, and survival. The longitudinal design, deep immunophenotyping, and large cohort are significant strengths. Using various statistical models, the authors found leukocyte, neutrophil, and monocyte counts increased gradually over time as ALSFRS-R score declined. Within lymphocyte subpopulations, increasing natural killer cells and Th2-diffrentiated CD4+ central memory T cell counts correlated with a lower risk of death. Increasing CD4+ effector memory cells re-expressing CD45RA T cell and CD8+ T cell levels associated with a higher risk of death. These findings have broad implications for ALS pathogenesis and the development of immune-based ALS therapies tailored to specific immune cell populations.
Thank you for the very positive comments.
-

Evaluation Summary:
Cui et al. colleagues carried out a longitudinal analysis of blood cell counts in a cohort of patients with ALS patients. They found increased numbers of neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not with rate of disease progression. In addition, increased levels in NK and central memory TH2 T cells correlated with a lower risk of death, while increased levels of CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death. These findings have broad implications for ALS pathogenesis and the development of immune-based ALS therapies tailored to specific immune cell populations.
(This preprint has been reviewed by eLife. We include the public reviews from the reviewers here; the authors also receive private feedback with suggested changes to the manuscript. …
Evaluation Summary:
Cui et al. colleagues carried out a longitudinal analysis of blood cell counts in a cohort of patients with ALS patients. They found increased numbers of neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not with rate of disease progression. In addition, increased levels in NK and central memory TH2 T cells correlated with a lower risk of death, while increased levels of CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death. These findings have broad implications for ALS pathogenesis and the development of immune-based ALS therapies tailored to specific immune cell populations.
(This preprint has been reviewed by eLife. We include the public reviews from the reviewers here; the authors also receive private feedback with suggested changes to the manuscript. The reviewers remained anonymous to the authors.)
-

Reviewer #1 (Public Review):
Cui and colleagues have performed a longitudinal analysis of blood cell counts in a cohort of ALS patients. The major findings include increases in neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not disease progression rate. Increases in NK and central memory TH2 T cells correlated with a lower risk of death, while increased CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death.
Strengths of the study include the sample size and effort to broadly include data.
Limitations of the study include indication bias, as the authors acknowledge, because the timing of the blood draws is not predefined. The specific review for possibility of infection does not, in this reviewer's opinion, sufficiently address this potential for bias. Also concerning is the …
Reviewer #1 (Public Review):
Cui and colleagues have performed a longitudinal analysis of blood cell counts in a cohort of ALS patients. The major findings include increases in neutrophils and monocytes that negatively correlated with ALSFRS-R score, but not disease progression rate. Increases in NK and central memory TH2 T cells correlated with a lower risk of death, while increased CD4 CD45RA effector memory and CD8 T cells were correlated with a higher risk of death.
Strengths of the study include the sample size and effort to broadly include data.
Limitations of the study include indication bias, as the authors acknowledge, because the timing of the blood draws is not predefined. The specific review for possibility of infection does not, in this reviewer's opinion, sufficiently address this potential for bias. Also concerning is the fact that half the subjects have only a single measurement, and how well the findings generalize to more or late measurements is not clear. Similarly, the number of later measurements driving some of the main findings is much lower, further raising concern about the potential bias. Given these issues, one really would want to see disease controls, and how the different cell counts change in another disease. Finally, there is not discussion about how or whether treatments, or changes in treatment, could influence observed counts.
-

Reviewer #2 (Public Review):
Cui et al. investigated the correlation of immune profiles in ALS patients to functional status (by ALSFRS-R score), disease progression (rate of ALSFRS-R decline) and/or risk of death (or invasive ventilation use). The study longitudinally assessed basic immune profiles from a large cohort of ALS patients (n=288). Additionally, they deeply immunophenotyped a subset of ALS patients (n=92) to examine immune cell subtypes on ALS status, progression rate, and survival. The longitudinal design, deep immunophenotyping, and large cohort are significant strengths. Using various statistical models, the authors found leukocyte, neutrophil, and monocyte counts increased gradually over time as ALSFRS-R score declined. Within lymphocyte subpopulations, increasing natural killer cells and Th2-diffrentiated CD4+ central …
Reviewer #2 (Public Review):
Cui et al. investigated the correlation of immune profiles in ALS patients to functional status (by ALSFRS-R score), disease progression (rate of ALSFRS-R decline) and/or risk of death (or invasive ventilation use). The study longitudinally assessed basic immune profiles from a large cohort of ALS patients (n=288). Additionally, they deeply immunophenotyped a subset of ALS patients (n=92) to examine immune cell subtypes on ALS status, progression rate, and survival. The longitudinal design, deep immunophenotyping, and large cohort are significant strengths. Using various statistical models, the authors found leukocyte, neutrophil, and monocyte counts increased gradually over time as ALSFRS-R score declined. Within lymphocyte subpopulations, increasing natural killer cells and Th2-diffrentiated CD4+ central memory T cell counts correlated with a lower risk of death. Increasing CD4+ effector memory cells re-expressing CD45RA T cell and CD8+ T cell levels associated with a higher risk of death. These findings have broad implications for ALS pathogenesis and the development of immune-based ALS therapies tailored to specific immune cell populations.
-